Sciatica
Sciatica is one of the most common , and also one of the most commonly misdiagnosed, pain conditions. Learn how to properly identify, and how to effectively address it.
Robert Inesta
1/30/202510 min read
Sciatica is an extremely common condition that affects millions of individuals worldwide, but also one of the most common misused and misunderstood terms I hear in practice.
As a clinician specializing in treatment of the nervous and musculoskeletal systems, I’d like to do a deep dive into the nature and causes of sciatica, clarify the common misconceptions around it, and share with you effective solutions.
True sciatica, or sciatic pain, is characterized by pain that radiates along the path of the sciatic nerve. The pain can begin in the lower back or buttocks, and travel down the back and/or lateral side of the thigh and below the knee into the leg, ankle and foot.
The pain is often sharp, shooting, burning or electric in nature. It can present with accompanying symptoms such as numbness, tingling (paresthesia), muscle weakness, and in more severe cases atrophy and even difficulty with bowel or bladder control.
The defining characteristic of sciatica is the radiating pain down the thigh and leg. One of the most common mistakes is that all localized pain in the lower back or even the buttocks are called sciatica, and this is not the case.
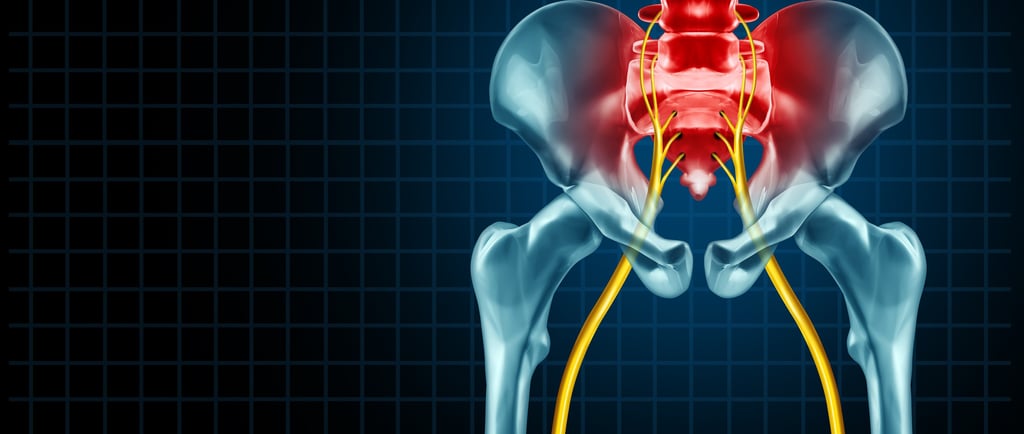
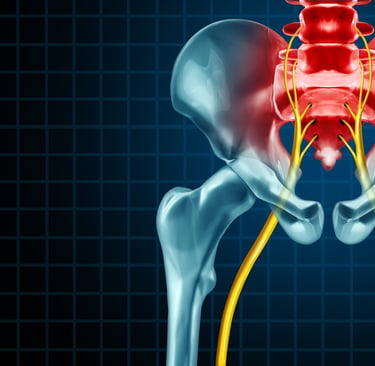
To understand sciatica better, it helps to have a basic understanding of the anatomy of the sciatic nerve and its course. It is the largest nerve in the body and composed of nerve roots that originate from the spinal cord in the lumbar and sacral regions (L4-S3). There is one on the both the right and left side of the body. It travels through the pelvis and down the back of the thigh. It branches out in the lower thigh before running down into the leg/calf to innervate the muscles and skin of the lower leg and foot.
What Causes Sciatica
Any irritation or compression of the nerve roots or nerve can lead to the symptoms we recognize as sciatica. This is what’s commonly referred to as a “pinched nerve” although that’s a term that’s not completely accurate. The causes of sciatica can be varied, and while many of them are commonly known, others are often overlooked. Here are the primary contributors to sciatica:
Herniated or Bulged Discs: One of the most common causes of sciatica is a herniated or bulged disc in the lumbar spine usually at the levels of L4/L5 and/or L5/S1. Discs are structures made of cartilage in between the vertebrae, and when they degenerate or become herniated or bulged, their inner gel-like material can protrude, causing inflammation and irritating the surrounding nerve roots.
Spinal Stenosis: This condition occurs when the spinal canal narrows, creating pressure and irritating the spinal cord and nerve roots. This narrowing, often associated with aging, can be caused by degeneration (arthritis) in the spinal joints and degeneration in the discs, causing significant discomfort. When the spinal joints degenerate, more bone will form which then reduces the amount of space in the canal where the nerves sit. If there is protruding disc material, it will further close down the space.
Spondylolisthesis: This condition arises when a vertebra slips forward or backward slightly out of place, which can lead to nerve compression. It can result from degeneration, developmental issues, or stress fractures in the vertebrae.
Piriformis Syndrome: The piriformis muscle, located in the buttocks, can tighten and compress the sciatic nerve, causing sciatica symptoms. This condition is often misdiagnosed, as it does not originate in the spine. The piriformis is considered an external rotator muscle of the hip. There are other external rotator muscles close to the piriformis that can have the same effect on the sciatic nerve causing symptoms as well.
Peripheral Nerve Entrapment: Like in piriformis syndrome, the sciatic nerve can become impinged by other muscles, fascia, ligaments and bones in the pelvis and thigh. Adhesions and tension caused by trauma or repetitive strain can develop between the fascia, muscles and nerves, causing the nerve to be “stuck” and inhibiting its ability to slide or move easily. This will cause the nerve to be stretched when attempting to move, which is irritating and painful. Other structures in addition to the piriformis and external rotator muscles that can cause entrapment are the sacrotuberous ligament, gluteus medius and hamstrings.
Injury or Trauma: Acute injuries, such as falls or accidents, can lead to direct trauma to the back and/or pelvis, resulting in sciatica symptoms. An impact injury can cause what’s known a crush injury to the sciatic nerve. Acute injuries can also cause herniated or bulging discs, nerve entrapments and spondylolisthesis.
Cysts, Tumors or Infections: While rare, tumors or infections in the spine can affect nerve roots and produce similar symptoms. Tumors can be malignant (cancerous) or benign. Cases that involve infection or malignant tumors require immediate medical attention. Cysts or other benign masses, while not as dangerous as cancerous masses, can create persistent problems and still require medical intervention.
Neuroplastic Pain: This is a chronic form of pain in which the affected tissue has healed but the neurological pain pathways have been so conditioned to activate that the pain sensation persists even when it there’s no physical reason for it. It can be difficult to treat because healthy movements that should not trigger pain still do. Mental stress and mindset play a large role in this.
Contributing Causative Factors
The most common causes of sciatica - herniated or bulged discs, stenosis and peripheral entrapment - in the absence of an acute trauma, are typically caused by lifestyle and repetitive unhealthy habits. These factors are cumulative with effects adding up over time. Here are common factors that can lead to the above conditions:
Poor posture and incorrect lifting/bending mechanics can create strain on the lumbar spine and soft tissues which will eventually lead to the above conditions.
Repetitive strain from physical work or sports, without appropriate stabilization, stretching and mobility work.
Sedentary lifestyle can lead to deconditioning and weakness in the core and stabilizing muscles of the spine and pelvis making it more vulnerable to injury.
Obesity is usually associated with sedentary lifestyle and is an indicator of inflammation, which can contribute to and worsen the situation.
Underlying medical conditions such as diabetes can negatively affect nerve health, creating complications and inhibiting the healing process.
Mental/emotional stress can have a massive impact on spinal and nerve health leading to fascial and muscle tension, inflammation, and neuroplastic pain.
Commonly Misdiagnosed
Despite an increasing awareness of sciatica, numerous misconceptions persist about its nature, causes and treatment. These concepts are crucial for both patients and practitioners to understand in order to address the problem in the most effective way.
The most common misconception, as we’ve already pointed out above, is what sciatica actually is. It is pain caused by irritation to the sciatic nerve, which radiates down the course of the nerve starting either in the lower back, buttock or thigh, and running down below the knee into the calf and/or foot. It can also have numbness or tingling and muscle weakness associated with it.
It is not localized low back pain or localized buttock or hip pain, as it is commonly referred to as. There are many causes of low back, pelvic and hip pain that don’t involve the sciatic nerve including muscle strain, spasm, fascial tension, joint sprains, disc derangement, arthritis, etc. Sometimes herniated discs can cause local back pain without irritating the nerve(s).
Additionally, sciatica-like symptoms can also be caused by trigger points mainly in the gluteus minimum muscle, but also in the gluteus medius and piriformis muscles. These trigger points, when activated, can produce radiating pain in the same areas as sciatic pain, but have nothing to do with the nerve. This is called pseudosciatica, or fake sciatica.
Another type of nerve pain commonly mistaken for sciatica is pain caused by irritation to the posterior femoral cutaneous nerve (PFCN). This is a small sensory nerve that exits the sacral plexus and innervates the lower buttock and back of the thigh. It’s different from the sciatic nerve in that it does not innervate muscles, and it’s sensory region is above the knee only. So if it were PFCN pain, it would not travel below the knee and there would be no muscle weakness or reflex changes associated with it. The pain would be anywhere from the lower buttock throughout the back of the thigh.
To be clear, sciatic pain doesn’t have to have muscle weakness associated with it, but it can. It can be purely sensory as well, but it will often present below the knee.
Other Common Misconceptions
Misconception: Sciatica is a Diagnosis
Many people use the term “sciatica” to describe any kind of lower back pain or hip pain. In reality, sciatica is a symptom of an underlying issue with the sciatic nerve and not a diagnosis itself. Identifying the precise cause is essential for appropriate treatment.Misconception: Sciatica Always Means Nerve Damage
While sciatica involves nerve irritation, it does not necessarily imply permanent nerve damage. In most cases, symptoms can resolve 100% with conservative treatment. However, ongoing symptoms may require further evaluation. Cases involving muscle weakness, atrophy and reflex changes raise the level of concern. Cases that involve bowel or bladder control issues are more severe and require medical intervention.Misconception: Surgery is the Only Treatment for Sciatica
Many patients fear that they will need surgery to overcome sciatica, and this is simply not the case. While surgical intervention may be required in some severe cases, the vast majority of people suffering with sciatica will not need surgery. In fact, most individuals respond well to conservative treatments, including chiropractic, acupuncture, physical therapy, exercise therapy and lifestyle modifications.Misconception: Sciatica Only Affects Older Adults
While age is a risk factor for degeneration, sciatica can affect individuals of all ages. Young adults, particularly athletes and people with physically intensive jobs, are also susceptible to sciatica due to activities that strain the lower back. Poor posture among the younger population due to smart phones and computers are also making them more susceptible to injury.Misconception: Rest is the Best Solution
Though rest may be beneficial for acute conditions, prolonged inactivity can worsen sciatica and the conditions that cause it. Controlled movement and therapeutic exercises, as advised by knowledgable professionals, are essential to facilitate healing, alleviate symptoms and prevent recurrence.Misconception: Exercise is Dangerous
This goes along with the above point, but importance cannot be overemphasized. While certain movements can aggravate sciatica, basic movement and specialized strengthening exercises are extremely beneficial and necessary. Consulting a professional is important in order to help make a plan and progress appropriately, as every individual is different with different needs.Misconception: All Sciatica Symptoms are the Same
Symptoms of sciatica can vary widely. Some individuals experience mild discomfort while others suffer from debilitating pain. In some cases, it’s purely sensory, whereas in others there’s a motor component (muscle weakness or atrophy) which is even more concerning. Symptoms also differ based on the root cause, which emphasizes the need for personalized assessment and treatment.
What To Do About It
Sciatic pain intensity can range from mild and annoying to severe and debilitating. The good news is that sciatica is treatable with natural conservative methods and completely reversible in most cases.
If you’re suffering with sciatic pain or what you believe to be sciatic pain, the first step is to determine what exactly it is. It’s always a good idea to seek the help of a professional who’s well versed in diagnosing and treating sciatic pain, such as a chiropractor, acupuncturist, physical therapist, orthopedist, physiatrist or neurologist.
A thorough evaluation is necessary to determine the cause of pain, determine which tissues are involved and why so that treatment can be precisely targeted. This is done through taking a detailed history and performing a physical exam. In some cases, advanced diagnostic testing such as MRI and EMG/NCV can be helpful. MRI, or magnetic resonance imaging, gives an anatomical picture of the region, showing bone and soft tissue such as discs, nerve structures and muscle/tendons. EMG/NCV, or electromyography/nerve conduction velocity test, is a physiological test that demonstrates the function of the nerves and the presence of any deficits.
If the source of nerve insult is a lumbar disc, then spine sparing, McKenzie and lumbar stabilization exercises are key. In some cases of stubborn herniated or bulging discs, decompression or traction therapy can be helpful.
If the source is more peripheral, meaning a nerve entrapment at the piriformis or other muscle, releasing tension in the muscles and fascia will be a key component. Soft tissue techniques such as Stecco Fascial Manipulation and Active Release Techniques (A.R.T.) are great for this and also for working the entire course of the nerve to assure the nerve can slide effectively through its surrounding tissues. These techniques are often provided buy chiropractors who have gone through additional training and certification. some physical therapists may also provide these services.
In both cases, acupuncture is extremely helpful for regulating the nervous system, releasing tension and reducing associated spasm in the muscles, pain control, and improving function of the nerve.
In some severe stubborn cases, oral anti-inflammatory medication and/or injections can help to break the pain cycle. Surgical interventions are usually only warranted in extreme situations when neurological deficit, such as loss of bladder/bowel control and/or muscle atrophy is present or in the case of a tumor or infection.
Whether the cause of sciatic pain is disc related, peripheral nerve entrapment, or stenosis, the following basic treatment principles will apply. The underlying condition will indicate specific details and focal points, but the foundational concepts are the same.
Implement spine-sparing exercises and habits such as McGill microbreak and hip hinge.
Walking, especially in the early morning upon waking, is one of the best exercises. Optimal distance and time will vary based on the individual situation and tolerance levels.
Mobilize the hips with soft tissue techniques such as Fascial Manipulation and Active Release Techniques (A.R.T.). Releasing tension from the fascia and muscles will allow the joint to move easier.
Stabilize the spine with exercises such as Stuart McGill’s Big Three (bird dog, curl up, side bridge).
Nerve flossing/gliding exercises to restore mobility to the nerve and keep it moving freely between the soft tissues and bones.
Reduce inflammation by avoiding inflammatory foods such as processed foods with unnatural additives, added sugar. Consider possible supplementation with omega 3 fatty acids, proteolytic enzymes and anti-inflammatory herbs if appropriate. Consult with a professional before adding supplements especially if on prescription medication.
Reduce and manage stress as much as possible. This is often an overlooked aspect of physical pain. Be mindful of chronic daily stressors and make changes accordingly. Consider major stressful events that may have happened around the time of pain onset. Seek professional help to work through this if necessary.
Address neuroplastic pain if present with Pain Reprocessing Therapy or other forms of psychotherapy that can target chronic pain.
Conclusion
Sciatic pain is very much treatable without drugs or surgery and does not have to take over your life. Some rare cases may need more aggressive medical or surgical interventions, but this is not the norm.
There are many factors that play a role in the severity of the condition, so a thorough history and exam is essential. Correct diagnosis is important in order to most appropriately target the underlying root cause and achieve optimal results.
There is much you can do to take action on your own and working with a knowledgeable practitioner who understands how to diagnose and treat sciatic pain will help guide you to achieve the best results as efficiently as possible. Most importantly, as always, know that you have the power to heal!
Want practical tools you can start using today?
Many cases of sciatica are influenced by posture, breathing, and movement pattern imbalances. I’ve created a free 10-day email and video series with simple practices to help you build a strong, resilient foundation for movement. Get the free series here.
Stress can play a major role in pain. If it's affecting you, you may also find this helpful: Stress Relief Guide.
Berkshire Functional Chiropractic & Acupuncture
FREE RESOURCES
info@berkshirefunctional.com
(413) 274-7161
© 2024. All rights reserved.
